Managing Different Ailments
Chronic diseases have an effect on all countries, and the augment in their prevalence is to a great extend attributed to varying demographics, improved life expectancy, changing lifestyles, better disease management and management and a better understanding of the factors that cause poor health and disease.
Laboratory, clinical and population-based research has revealed that a few risk factors are responsible for the prevalence of most chronic diseases:
unhealthy diet and high energy ingestion, lack of physical activity and use of tobacco. Alcohol intake, environmental pollutants, age and hereditary factors also play a role. These risk factors are the same in men and women and across all regions in the world.
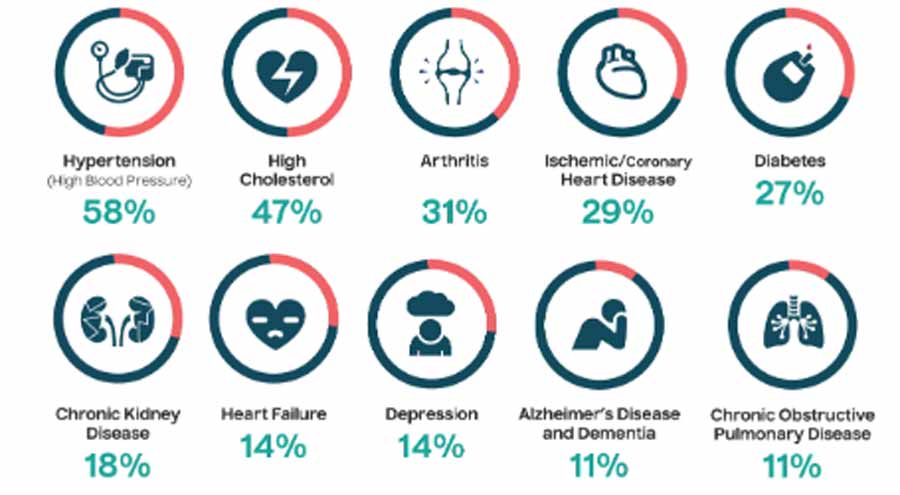
The associated healthcare, financial and social burden of chronic diseases, which include diabetes, coronary heart disease, asthma, chronic obstructive airway disease, hypertension, chronic depression, osteoporosis, end stage renal failure and stroke, are progressively on the increase.
Also Read:
- Discover Your Baby’s Personality
- Kitchen Activities: Ensuring Efficiency and Quality in Managing
- Small But Useful Tips for General Ailments
- Be Aware of Computer Generated Diseases
- Secret of Your Health Lies in the Way You Sleep
Table of Contents
Managing Different Ailments
In clinical circles, managing different ailments can be defined as an elaborate, systematic, multi-component strategy to delivering healthcare while involving all members in the population or community who suffer from similar infections.
Cardiovascular disease is serious and is the first cause of death among the elderly in all countries. Studies show that even 60 years ago, ailments of circulatory system and pneumonia were the first causes of death among the aged in Jamaica in 1950.
As life expectancies are increasing the prevalence of all non-communicable disease is also increasing. Thus, one could adopt the approach that these are a foreseeable consequence of ageing and the focus, therefore, has to be on simply treating them when they do occur and applying the acknowledged interventions for secondary prevention once the first disease episode has occurred.
It is possible to reduce the mortality from chronic diseases in general. Some of the developed countries such as Canada, Australia and the United States have succeeded in reducing mortality by applying preventive measures. Managing different ailments has been known to be the best and most comprehensive approach for providing holistic care for patients with ailments.
The Kaiser Permanente Care Triangle has frequently been used to conceptualize disease care at three main levels:
- Supporting self-care for patients suffering from chronic disease who are at low risk of complications and hospitalization.
- Disease management for people who are in need of regular routine follow-up and are at high risk of chronic disease.
- Case management for people who have complex needs and those who are high-intensity users of unplanned less important care.
Managing serious ailments means focusing on the need to reorganize care delivery to meet the healthcare demands of populations of patients who suffer from chronic illnesses.
In October 2001, both the British Medical Journal and the Western Journal of Medicine published special issues focusing on the problem of serious ailments and hinted how various nations are dealing with this ever-rising epidemic.
It is, therefore, timely that all nations focuses on coming up with a better program to address the needs of patients with chronic disease, on the advances in clinical and non-pharmacological management, and the challenges faced in ensuring that patients receive optimal care meeting the needs at the various stages of their disease.
A successful ailment management program should be designed while considering fundamental factors that are critical to its sustainability. First of all, the program should be aimed at a certain specific condition within the population suffering. Then the next important factor concerns the availability of evidence on which its functions should be based.
A good program has to keep in its consideration the existence of obstacles which may be a hindrance to its successful implementation. Adequate measures should be put in check to ensure that there is a balance between quality and the economics of the objectives of care to be given.
According to statistics in the United Kingdom, lack of proper care to manage different ailments on a day-to-day basis can lead to unnecessary complications and premature death. Children below five years account for 15% of the cases (General Household Survey, 2002).
Self care has sometimes been ignored in the UK but it is a well-proven approach to improving the situation of chronic diseases. Self-care or managing different ailments is not just an issue of providing information to the patients but it involves a range of other things to make it workable.
Patients need care education regarding self management of their sickness by helping stand what they ought to do and how to make adjustments towards their medical dosage and how and when they need healthcare. They also need quick reminders of when they should be attending to certain measures concerning their health.
They need support from knowledgeable patients or even an expert in their disease and broader networks which can include attending to group practices involving the same kind of health condition.
Their uncertainty regarding self-care, however, it is likely to improve in relevance because of the following:
- The increase of information that is availed to the patients.
- The ability of information technology to support self-care.
- The possibility of having reliable and accurate home monitoring systems.
- The greater anticipation by many patients to be the locus of control.
Future of ailment management programs
Evidence that has been observed throughout the world brings out clearly that, to be successful, policy-makers should put into consideration:
- Providing well-built leadership and vision at the national, regional or organizational-level, which should oversee all that is required for the programs to succeed.
- They should ensure full-bodied collection of information and data-sharing among all the stakeholders in health sector.
- Care should be provided based on people’s needs and an ability to identify people with different levels of need.
- They should also put in place measures that target key risk factors, including widespread disease prevention initiatives.
Future ailment management programs should be tailored to reduce the costs associated with care for people suffering from chronic illnesses. The growing costs of operations such as dialysis are still a major concern in most countries. But with such programs in place, these costs are expected to decline and lead to improved care even through public health for cases of different ailments.